WHAT IS THE MICROBIOME?
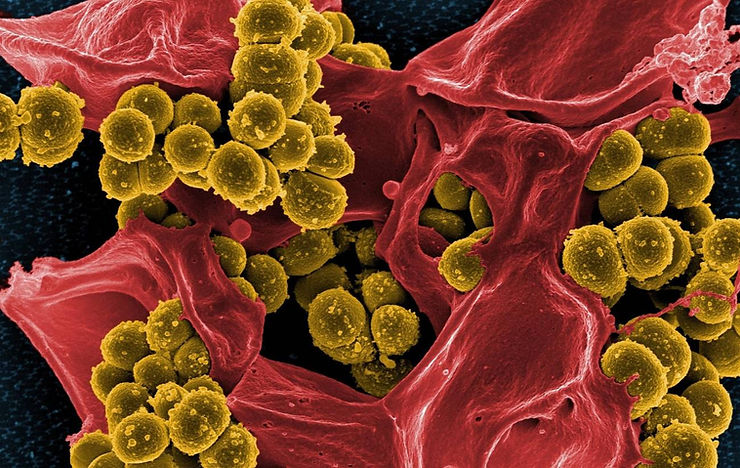
About 10 million bacteria, fungi, and other microbes live in and on us, mostly in the gut, though they are also in the mouth, on the skin, and almost everywhere else in the body. They far exceed human cells in quantity, raising questions about whose body the body belongs to. For decades, this population called the “microbiome”, has been considered to be primarily a potential source of infection.
However, recently scientists discovered that the microbiome is indispensable to human life because, for example, it helps with nutrition by digesting what the body is unable to do on its own and extracting a few more nutrients and calories from the meal. More mysterious, however, is that the microbiome intertwines with the immune system, supporting health in unexpected ways. Together they maintain the mucosal lining that protects the body’s organs against microbial invasion and are involved in suppressing or eliminating harmful and troublesome bacteria.
The microbiome tests and trains the immune system, while the immune system takes care of the microbiome.
“Those bacteria are not there by chance. We grow with them from the moment we are born and throughout their development, they help our immune systems mature throughout the body, but especially in the gut,” says Mayo Clinic gastroenterologist and researcher Dr. Joseph Murray.
THE RELATIONSHIP OF THE MICROBIOME AND AUTOIMMUNE DISEASES
Recently, Dr. Murray and other Mayo Clinic researchers discovered an association between microbiome imbalance, a condition known as “dysbiosis,” with autoimmune diseases such as rheumatoid arthritis, multiple sclerosis (MS), and celiac disease. It is not known whether dysbiosis is the symptom or the cause of the disease, but work has shown that a type of bacteria native to the microbiome, known as Prevotella cisticola, could be the key to getting the microbiome back on track and alleviating some effects of these autoimmune diseases.
Dr. Murray baptized Prevotella histicola with the nickname “brug”, due to the mixture of the English words for “bug” (bug) and “drug” (drug).
Multiple sclerosis, rheumatoid arthritis, and celiac disease are common autoimmune diseases that occur when the body’s immune system, which is meant to destroy invading organisms, overreacts and attacks the body’s tissues.
In multiple sclerosis, the immune system breaks down the protective myelin sheath that covers nerve fibers, causing symptoms such as numbness, weakness, and vision loss. In rheumatoid arthritis, the target is the joint, mainly the synovial membrane, which causes inflammation that can lead to erosion. In celiac disease, eating gluten triggers a misguided immune response that damages the lining of the small intestine, leading to diarrhea, weight loss, bloating, and anemia.
“The fascinating observation that has been made in the last 10 years is that all of these diseases have what is known as dysbiosis. As the bacteria discovered in the gut is different from that found in healthy control subjects, something is up with the gut bacteria, but… Is it the consequence of the autoimmune disease or is it its cause? That’s the crux of the business we’re at,” says Eric Marietta, MD, a Mayo Clinic gastroenterology researcher.
The incidence of autoimmune diseases is increasing in developed countries, but it is not known why. One approach is the “hygiene hypothesis”, that is, with the cleanliness of the environment in which we live and as we work even harder to expel or eliminate bacteria, our immune systems have less exposure to microbes and less work to do.
“In this, some apply the analogy that ‘idleness is the mother of all vices,’ with the idea that an immune system that is idle (because it has little to do) can go astray and that, in general, we need certain things, especially the microbes that live inside and outside of us, to help us maintain a relationship. The microbes stimulate the immune system a bit so that we have good defenses, but they also help suppress or check the immune response,” says Dr. Murray.
STUDIES AND TESTS
Mayo Clinic immunologist Dr. Veena Taneja comments: “I came to Mayo because of the mice. Specifically, I wanted access to genetically engineered mice to create a facsimile of human rheumatoid arthritis. Did they have different gut microbiomes than mice without the disease? That was the question I wanted to find an answer to”, says Dr. Taneja.
In collaboration with Dr. Murray, Dr. Taneja discovered that dysbiosis of gut bacteria in rheumatoid arthritis mice played “an important role for gut flora” in the development of the disease.
Drs. Taneja, Murray, and Marietta, along with other Mayo researchers, identified Prevotella cisticola as a microbe with possible “immune system effects.” Mice in Dr. Taneja’s lab were given rheumatoid arthritis by human arthritis-related genes and treated with billions of oral doses of Prevotella cisticola for several weeks. The dose is not as big as it seems, because up to 6 billion bacteria fit in the mouth at any given time.
Mice treated with Prevotella cisticola showed “significantly lower incidence and severity of arthritis, compared to control group mice.”
“Even though I did it myself, I didn’t believe it. How was it possible that just giving the bacteria to mice stopped rheumatoid arthritis in 50 percent of them? Therefore, I repeated the test for the second time… for the third, for the fourth, and for the fifth time. The strain [of Prevotella histicola ] controls the immune system and the intestine,” says the scientist.
At this point, the obvious question was how. The microbe reduces the body’s immune response, not only in the gut but also throughout the body, and increases the activity of regulatory T cells that modulate the immune response and influence dendritic cells, which present antigens to immune cells to initiate the immune response. Prevotella histicola also counteracted leaky gut and blood-brain barrier, which are characteristic of patients with autoimmune diseases. Similarly, it seems to restore some normality and stability to the microbiome, reducing the chemical signals that trigger inflammation. These results were published in 2016 in Genome Medicine.
The researchers tried a similar experiment using mice engineered to show multiple sclerosis. In the study, published in 2017 in Cell Reports, Prevotella histicola showed a similar ability to suppress the body’s immune response and slow both the symptoms and progression of multiple sclerosis.
But how can a single organism achieve all this? Does it do this by directly regulating the cellular response, through the production of byproducts that suppress the immune response, through the regulation of other microbes to bring the microbiome into the normal range, or by all of these means? This matter is still a mystery.
However, researchers are working on another similar study for the treatment of type 1 diabetes. Mayo Clinic patented the use of Prevotella cisticola to treat these autoimmune diseases and has just started the first clinical trials.
If the trials are successful and Prevotella cisticola exerts the same effect in humans as it does in mice, this could lead to new therapies for people with autoimmune diseases. Restoring the balance of the microbiome and alleviating symptoms could be as easy as taking pills with Prevotella cisticola. “If my immune system resists the colonization, I can continue taking them; but if you accept colonization, you may not have to take them for life,” adds Dr. Taneja.
While genetics play an important role in shaping the microbiome, patients can take steps to improve the likelihood that their microbes will remain healthy, diverse, and stable.
“One of those measures is to feed them good food. In this, it seems that the vegetarian diet is healthier than the diet based on meat and fat. The second measure is not to take antibiotics, unless you need them, because taking them is equivalent to putting an atomic bomb in the microbiome”, concludes Dr. Murray.